What is Diabetic Retinopathy?
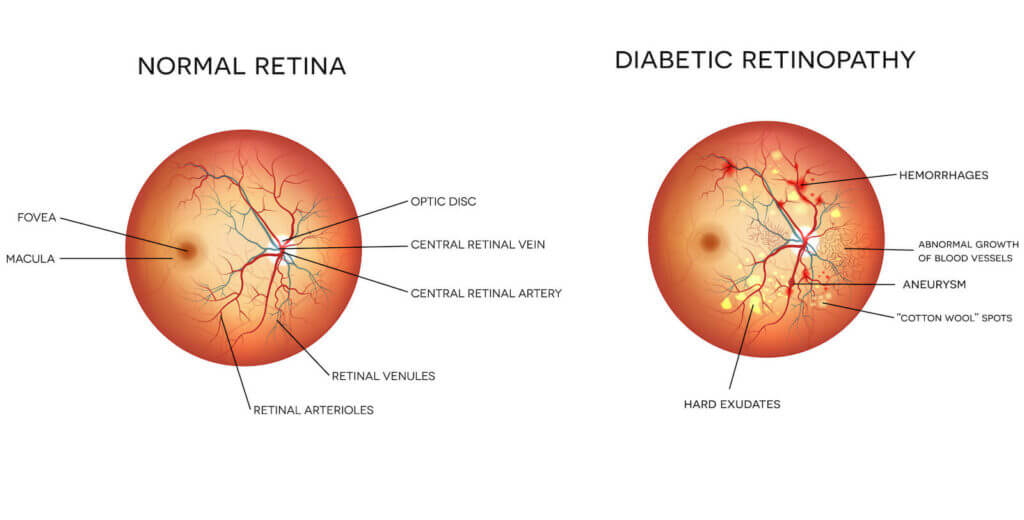
The layer of nerves at the back of your eye that connects to the brain to create pictures is called the retina. Any disease of the retina is called retinopathy. It’s very common with people with diabetes, giving the name of diabetic retinopathy. It can lead to a decrease in vision and even blindness, with no symptoms when the disease first begins. At Spectrum Eye Physicians we have a wide variety of patients who were surprised with a diagnosis of diabetic retinopathy, only finding out the disease was progressing because of their regular eye examinations.
Symptoms of Diabetic Retinopathy
In the beginning, the blood vessels in the eye begin to weaken. Some will eventually break, leading to blood and other fluids leaking into the eye. This can lead to blurry vision, which is usually one of the very first symptoms of diabetic retinopathy. This usually only happens after the eye has sustained significant damage. In most cases, you won’t notice any symptoms until the disease has progressed significantly, which is why it’s so important to have your eyes examined frequently, especially if you have diabetes.
Diabetic Retinopathy Treatment
Researchers haven’t yet found a cure for diabetic retinopathy, but there are multiple treatments that will slow vision loss if done before too much damage has happened. Laser treatment is usually the most effective in preventing vision loss, especially in the first stages of the disease. Multiple medications can offer help in slowing down the progression of the disease.
The absolute best treatment possible is to control both your blood sugar and your blood pressure. Keeping these numbers within prescribed ranges will lower any chance of diabetic retinopathy from progressing and creating a loss of vision. Have your eyes examined every year if there are no changes in your eyesight, and come into our office right away if you have any significant change in your vision in between visits. Having one of our ophthalmologists screen your eyes for diabetic retinopathy won’t cure the disease, but early diagnosis is the only way to begin treatment early enough to help slow down or prevent damage to your eyes.
Contact Spectrum Eye Physicians Today!
Schedule your appointment online or call us at 408-884-2215. No matter which of our locations you visit, you will receive the latest in eye care technology from friendly eye doctors and staff committed to serving you.
Request Appointment